Remote patient monitoring, commonly referred to as RPM, has received a lot of attention lately. At the beginning of 2019, CMS released reimbursement codes specific to required RPM components and necessities for providing a solid program. This includes hardware and data, virtual clinical management of patients, and the education, onboarding, and compliance of patients.
Learn more about RPM reimbursement: Understanding CMS Reimbursement Opportunities for Remote Patient Monitoring.
According to a Deloitte paper, over the next 25 years, RPM is expected to save $200 billion in healthcare costs globally.
For the many stakeholders who stand to benefit, it is a good time to consider an RPM program. Organizations with population health initiatives and clinical teams benefit as they have historically absorbed the “between clinical visit” time to manage patients with chronic conditions. RPM is now a welcome addition to the traditional model of care. It is now a benefit to patient care.
In addition to CMS, the American Heart Association has also acknowledged the value that RPM brings to care. In an article, “Using Remote Patient Monitoring Technologies for Better Cardiovascular Outcomes Guidance,” the AHA highlights the benefits in the following point: RPM empowers patients, informs clinicians, and expedites intervention when necessary.
From the same article:
- Federal healthcare spending is approaching 20% of the GDP
- The cost to treat chronic diseases is 3.5 times higher than that of other conditions
- Chronic conditions account for 80% of all hospital admissions
How RPM Benefits Cardiovascular Disease Management |Clear Arch Health
On average, a hospitalization for congestive heart failure as a primary diagnosis is about a week in duration and the cost is more than $20,000. This is an example of one of the associated hard costs. Others include the penalty costs hospitals face when patients are readmitted. Soft costs are less documented.
However, as we consider the impact of managing an illness and a hospital occurrence to the individual patient and their families, we must consider how RPM might better relieve costs such as travel, lost wages, and caregiver stress.
According to a 2016 New England Health Care Institute study, RPM for a patient with congestive heart failure might result in a net savings of $5,034 per patient, per year when compared to standard care. We expect even greater savings to be reported in years to come.
RPM provides an affordable option for clinical teams to understand a patient’s status outside of clinical visits. It provides data that prioritizes patients when their health declines, speeding the time to intervene and manage the situation before it becomes unmanageable. Remote patient monitoring also supports population health initiatives as it informs clinical teams of which patients to prioritize within a group by symptom control, adherence, and survey response. The communication paths become proactive and care plans are reinforced at the time an issue arises.
While highlighting the cardiovascular outcomes to date, such as improved systolic and diastolic blood pressure with RPM, improved heart failure related outcomes, and the potential benefits with atrial fibrillation, the AHA suggests a need for more significant evidence yielded through long-term, large population clinical trials.
As attention is drawn to RPM programs, the healthcare community will benefit from our shared knowledge about ongoing programs. Overall, building programs can be a lot of work. It is important to note that qualitative and quantitative measures for the purpose of tracking outcomes must be included in the planning process.
One approach, when in the process of planning or redesigning a solid RPM program, is to include analytics to identify the right patient populations and meaningful metrics to ensure the program is successful. It is to everyone’s benefit that solid evidence is shared.
A health analytics company that provides such support is Versatile MED Analytics, a partner of Clear Arch Health, which offers additional insight into healthcare organization data. The company recommends:
Define the target audience based on clinical criteria, where the opportunities exist, and budget. Programs require data to substantiate the potential impact and prioritize where to start. From there, patient identification should begin with analysis to identify the total universe of people who could benefit from an intervention. However, it is likely that your program budget will not support engaging all of them through outreach and care delivery.
Therefore, it will be necessary to match the initial budget to a specific sector of patients where the data indicates they can realistically be reached and clinically impacted by your proposed program.
Start early during the planning stages to define desired outcomes and assign resources for tracking. Why? Because this will be your opportunity to:
1) Confirm what you want to track (your outcome or “measure of success”) is supported by existing data
2) Build data capture mechanisms, if necessary; and
3) Document baseline values which are key for demonstrating affected change after the program has been implemented
In short, choose your program goals and include the process to measure the outcomes before you implement. Some areas that can be measured include:
- Adherence, compliance
- Symptom improvements/decline
- Patient satisfaction
- Cost of care
- Travel costs
- Behavioral change
- Patient engagement/activation (PAM Scores)
The change in reimbursement has highlighted the value of RPM to the model of care. To support continued positive outcomes, the AHA suggests, “Future research should focus on understanding the process by which RPM works in terms of improving HF (heart failure) related outcomes, identify optimal strategies and the duration of follow-up for which it confers benefits, and further investigate whether there is differential effectiveness between chronic HF patient groups and types of RPM technologies.”
With solid partnerships in place, accomplishing such tasks is manageable as partners offer shared resources, intelligence and skills. Remember that innovation isn’t about invention – it’s collaboration and the leveraging of partnerships that can be the innovative solution. Building teams of healthcare organizations, vendors, consultants, and providers to design trials that include insight into all the areas can help make for a successful RPM program with measurable outcomes.
More about the partnership:
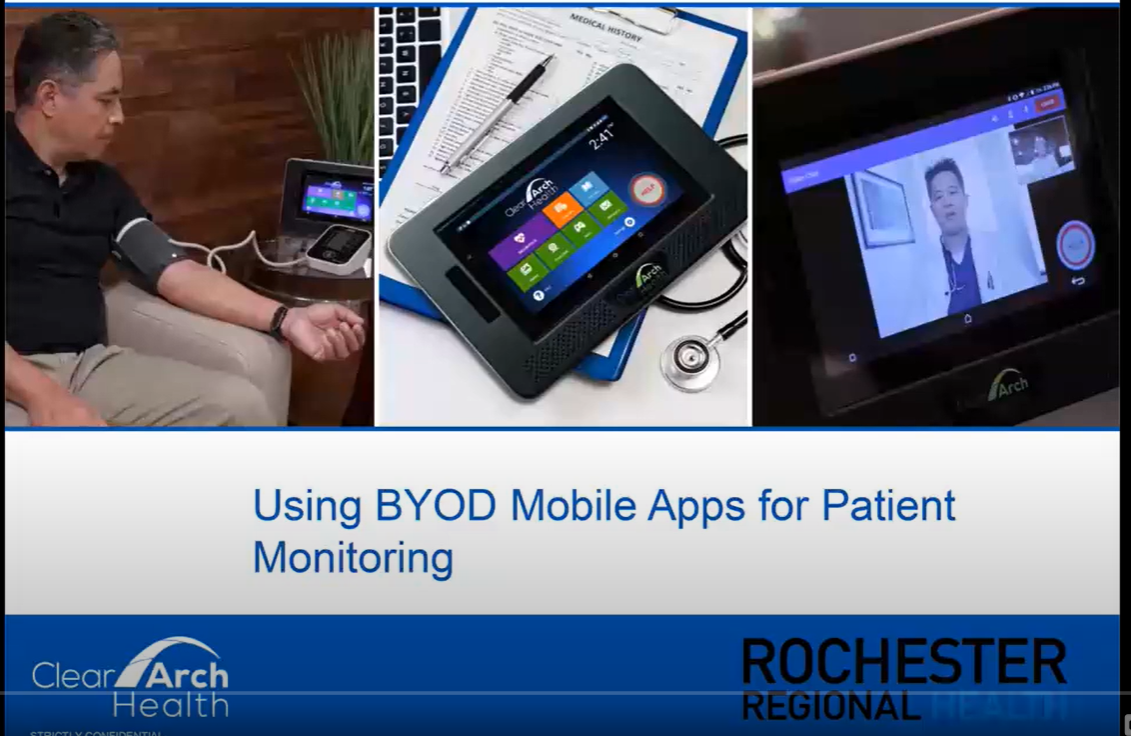
To deliver successful remote patient monitoring programs, Clear Arch Health provides options to our client partners. These options are both valuable and flexible, fitting our client partners’ specific program and population needs. In addition to offering exceptional hardware, clinical monitoring software, and a patient portal – Clear Arch Health also provides logistics, contact center services, integration and now – data analytics.
With a continued focus to improve patient-centric care and balancing organizational goals to reduce care costs, Clear Arch Health continues to expand services.
This is a joint blog by:

Published by: Lisa Levitt
Lisa Levitt writes about healthcare analytics, innovation and digital health. She is passionate about improving customer experience, measuring results and collaborative problem solving. Lisa is a thought leader at the intersection of business, analytics and technology. She is the Senior Director, Strategic Solutions and West Coast leader at Versatile MED Analytics, a healthcare analytics and data solutions company headquartered in Albuquerque, NM. To learn more, visit versatilemed.com. Also as Professor at the University of California Irvine, Lisa develops and teaches courses on Digital Health, Business Data Management, and comparative health care systems.

Published by: Jerriene Cordova
Jerriene Cordova is a healthcare executive with more than two decades of experience in developing new markets and building strategic alliances with patient-oriented organizations. Her areas of expertise include telehealth programs, remote patient monitoring, case management solutions and clinical research. Currently, Jerriene is the Director of Telehealth Programs at Clear Arch Health. Her extensive prior experience includes companies such as GlaxoSmithKline (GSK), Aflac, and Ideal Life and she is a member of the American College of Healthcare Executives. She holds a BS in Biology from the University of New Mexico and is currently pursuing her MBA from LSUS.